What is granuloma annulare?
Granuloma annulare is a benign skin condition characterised by smooth discoloured plaques which are thickened and annular (ring-shaped). It is relatively common in children and adults, although women have a slight increased risk. The several clinical variants of granuloma annulare include localised, generalised, subcutaneous and perforating. It often resolves spontaneously within a few years and granuloma annulare treatment is only indicated for patients with symptomatic cases or cosmetic concerns.
The exact cause of granuloma annulare is unknown. A number of potential causes have been suggested, including trauma, insect bites, sun exposure, medications and viral infections like hepatitis B, hepatitis C and HIV. A few studies have reported on genetic factors influencing the susceptibility to GA but the results were inconsistent. Mechanism of GA is a delayed hypersensitivity reaction to some components of the skin.
What are the symptoms of granuloma annulare?

The most common form is localised granuloma annulare which presents as skin-coloured or red, round and firm plaques with rope-like border and central indentation. It typically develops over the joints, such as the fingers, the backs of both hands, elbows and on top of the foot or ankles. This form of granuloma annulare is more common in children and grows slowly in a centrifugal pattern. Most cases are multiple lesions with less than 5cm in size.
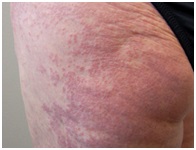
Another form is generalised granuloma annulare which is more common in adults. It presents as skin-coloured or pinkish patches with small bumps that are widespread. The lesions may be itchy in some cases and are more prominent in the trunk and limbs, especially the skin folds of the armpits and groin.

Subcutaneous granuloma annulare present as painless, rubbery nodules on the scalp margins, fingertips or shins. It is also located on the hands and buttocks of children. The skin overlying the nodules appears normal and are usually less than 4cm. The single or multiple lesions may be mistaken as rheumatoid nodules.
Perforating granuloma annulare is a variant in which damaged collagen is eliminated through the skin. The plaques presented are described as red bumps that evolve into yellowish, raised lesions with central umbilication. Commonly seen in children and young adults, it may be localised on the hands or widespread. The lesions can be painful and itchy, but eventually heal with scarring.
How is granuloma annulare diagnosed?
Granuloma annulare is a clinical diagnosis in which the recognition of classical symptoms are usually sufficient. A skin biopsy is useful when diagnosis is in doubt. Blood tests are not needed to diagnose granuloma annulare but may be useful to check for lipid profile, blood sugar and HIV in certain cases. Research found that granuloma annulare may be associated with dyslipidemia, diabetes and HIV infection.
How is granuloma annulare treated?
Granuloma annulare is often self-limiting within a few years and most cases do not require treatment. However, treatments are available for lesions that are painful, itchy, persistent or cosmetically distressing.
The first-line treatments for localised granuloma annulare are super potent topical corticosteroid or intralesional corticosteroid. For those who declined intralesional injections with triamcinolone, topical corticosteroid like clobetasol 0.05% cream or spray can be given. Apply once or twice daily for at least 2 to 4 weeks. Side effects include skin thinning, skin discolouration and visible tiny blood vessels. These medications are relatively safe with proper usage but patients should be followed up closely.
For patients with generalised granuloma annulare who desire treatment, topical calcineurin inhibitors and phototherapy with UVA1 are recommended due to the available evidence of their effectiveness and low side effects. Topical corticosteroid may be useful for selected lesions but should not be used throughout the body as it poses a risk to systemic side effects of steroids.






Comments